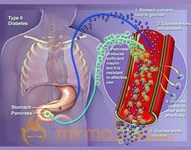
What it is: High blood sugar, technically known as hyperglycemia, can occur when a person's blood sugar stays too high -- typically over 180 milligrams per deciliter (mg/dL) -- for too long. High blood sugar is an indication that his body doesn't have enough insulin. It can happen if he skips doses of his diabetes medications, eats too much, or doesn't get enough exercise. Sometimes the medications he takes for other ailments cause high blood glucose. In addition, an infection, illness, injury, surgery, or stress can also make his blood glucose soar to harmful heights.
Symptoms:
Excessive thirst
Fatigue
Increased urination
Blurry vision
Nausea
More frequent infections
Slow-healing cuts and sores
Unexplained weight loss
How to treat it:
Make sure the patient drinks plenty of water to avoid dehydration (and the potential for high blood sugar to spiral out of control into an emergency situation). For specific details, see our article on emergency complications such as ketoacidosis.
If his blood glucose level is above 250 mg/dL, he should test his urine for ketones, acids that can build up in his body and cause the above-mentioned potentially life-threatening problems. Ketone test strips are available over the counter at pharmacies.
If his blood glucose readings are routinely above his target range, he may need to start taking pills or injecting insulin, if he doesn't already. Or he may need to increase the dose of either one of these medications. Discuss these concerns with his main diabetes care provider.
How to prevent it:
Help the patient figure out what foods may trigger a high blood-sugar reaction so he can avoid them or compensate by adjusting his medications or becoming more active.
Check his portion control to make sure he's not eating too much. Or enlist the aid of a certified diabetes educator or registered dietitian to see if too much food is the cause of his trouble.
Reassess his activity plan with him and his main diabetes care provider to determine if lack of exercise, or the timing of it, may be to blame.
Make sure he isn't skipping prescribed medication doses. If he uses insulin, check to see that it's not spoiled and he's taking the correct amount.
Clean his blood glucose meter and check to ensure it's working properly. Make sure his testing strips haven't expired and that they're calibrated for his device. Review his testing techniques with his care provider to ensure he's getting accurate readings.
If his glucose is frequently too high or he often experiences symptoms of high blood sugar, you and he should talk with his doctor. He may need a change in his diabetes medicines, meal plan, or other aspect of his self-care regimen.
What it is: This condition occurs when a patient's blood sugar level drops too low -- typically less than 70 mg/dL -- to provide enough energy for his body's activities. Older adults with type 2 diabetes are more prone to this condition than others with the disease and are harder hit by its potential consequences, such as driving accidents or injuries from falls.
Caught early, this situation can be quickly remedied. But left untreated, low blood sugar can lead to loss of consciousness. Hypoglycemia, sometimes referred to as an insulin reaction, can come on suddenly and may be a result of taking certain diabetes drugs designed to keep blood sugar levels under control, such as sulfonylureas. In addition, sometimes medicines taken for other conditions can cause blood glucose to dip to unhealthily low levels -- as can alcohol.
Symptoms:
Hunger
Nervousness or shakiness
Perspiration
Rapid heart rate
Dizziness, light-headedness, or headache
Sleepiness
Confusion or difficulty paying attention
Trouble speaking
Anxiety, weakness, or irritability
Sudden mood change, such as unexplained crying or antagonistic behavior
Clumsy or jerky movements, lack of coordination
Pale skin tone
If this condition occurs while a patient is sleeping, he may:
Cry out or have nightmares.
Find his pajamas or sheets damp from perspiration when he wakes.
Feel tired, irritable, or confused when he wakes.
How to treat it: Typically, hypoglycemia can be addressed by consuming a quick-fix, sugar-rich food such as:
3 to 4 glucose tablets
1 serving of glucose gel
1/2 cup (4 ounces) fruit juice
1 cup (8 ounces) of milk
1 to 2 teaspoons of sugar or honey
5 to 6 hard candies
Then follow the 15-15 rule: After 15 minutes, check a patient's blood sugar again to make sure it is 70 or above. If not, have him eat or drink a carbohydrate-dense food or liquid such as one of those listed above; each contains about 15 grams of carbs. Even if his numbers bounce back, if it's an hour or more before his next meal, give him a carb- and protein-rich snack, such as peanut butter toast or half a turkey sandwich.
If he's unconscious or unable to swallow, an injection of glucagon, a hormone that raises blood glucose quickly, may be necessary. Before an incident happens, ask his healthcare provider if this is an appropriate treatment and, if so, learn how to administer it. While you're giving the shot, someone else should call 911.
How to prevent it:
A patient can often prevent low blood sugar by eating regular meals and snacks. Make sure he gets enough food at meals and doesn't delay or skip eating.
He should test his blood glucose regularly so he can monitor if he's in his target range. Ask his primary diabetes care provider how often he should check and what his recommended range is.
If he takes diabetes medications that can cause hypoglycemia, make sure he always carries an emergency food or drink supply and wears an identification tag like those found at the caregivers know how to give a glucagon injection if necessary. Ask his main diabetes care provider for instructions in advance.
If his glucose is frequently low, or he often has symptoms of low blood sugar, call his doctor. He may need a change in his diabetes medications, diet, or some other aspect of his treatment plan.
Sometimes, for no apparent reason, low blood sugar occurs even when he's doing all he can to keep his blood glucose in check. In such cases, although you can't prevent it, the condition can be treated before it gets worse.
What it is: Hypoglycemia unawareness occurs when a patient has low blood sugar without any symptoms, or he's unable to recognize the early warning signs of this condition. In such cases, he could lose consciousness from low blood sugar without ever experiencing symptoms.
This acute problem is more common in people who have had diabetes for years and in older adults. That's because after about five years following a diabetes diagnosis, the symptoms of low blood sugar tend to fade. After 20 years with the disorder, sometimes symptoms are too subtle to detect, or they occur only after a patient's glucose level has gone too low for too long and he's unable to treat the condition himself. It's also more likely to occur if he has neuropathy (nerve damage) or if he takes certain heart or high blood pressure medicines.
Symptoms:
Often there are none, hence the name.
Sometimes while the physical and behavioral signs of low blood sugar aren't apparent, a patient may still detect mental red flags for the condition, such as difficulty concentrating, slowed speech, slowed thinking, or lack of coordination.
How to treat it:
If he's unconscious, call 911.
If he's unconscious or unable to swallow, and if he has a glucagon emergency kit and you or another caregiver knows how to use it, give him the injection.
Otherwise, call his main diabetes doctor and treat as for hypoglycemia.
How to prevent it:
Keep on the lookout for mental indications of low blood sugar the person you're caring for, and point them out to him so he can stay on top of his condition.
Make sure he checks his blood glucose on a routine basis.
Resources:
Acute Diabetes
2 Low Blood Sugar Hypoglycemia With Diabetes